Download Patient Toolkit
Additional Resources
- IBD Parenthood Project
- Get Your IBD Questions Answered
- What is an MFM?
- Find an IBD Doctor
- Connect with Others
New Online Resource from AGA and the IBD Parenthood Project, in Collaboration with Multidisciplinary Experts, Provides Guidance and Dispels Fears About Pregnancy for Women with IBD
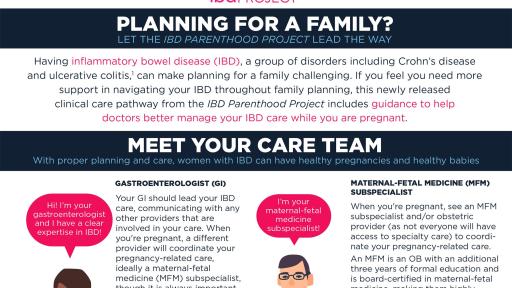
Downloadable toolkit educates around the proper planning and care required for healthy pregnancies and healthy babies
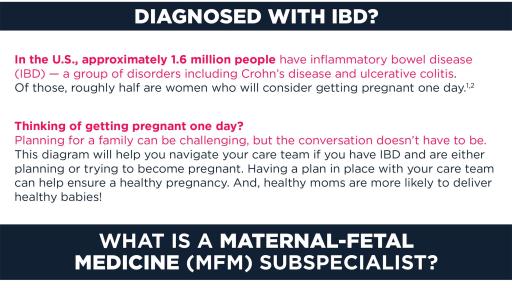
Bethesda, MD (Jan. 18, 2019) – The American Gastroenterological Association (AGA) has announced the launch of the IBD Parenthood Project and a new online resource, which aims to address misperceptions and fears women with inflammatory bowel disease (IBD) and their health care providers (HCPs) experience throughout all phases of family planning. This patient-directed initiative, which was created by gastroenterologists (GIs), maternal-fetal medicine (MFM) subspecialists and patients, is led by AGA with support from the Society for Maternal-Fetal Medicine, the Crohn’s & Colitis Foundation, and patient support network, Girls With Guts.
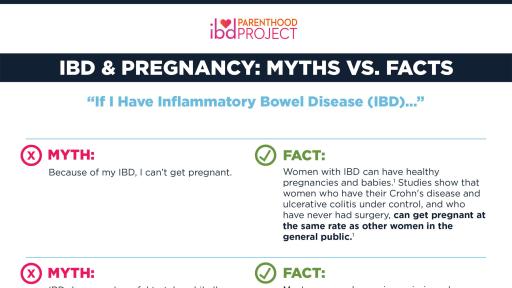
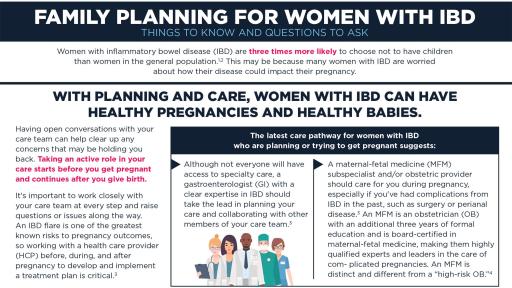
With proper planning and care, women with IBD can have healthy pregnancies and healthy babies. Unfortunately, many women with IBD decide not to have children based on misperceptions about their disease and pregnancy. In fact, a recent survey conducted by AGA of 286 women in the U.S. diagnosed with IBD who are trying to conceive, are pregnant or have had a child in the past 12 months revealed that 65 percent disagreed or were unsure that IBD medications were safe to use during pregnancy, and 57 percent have worried about medication harming their baby; yet over half rarely or never discussed their diagnosis with their obstetrician/gynecologist (OB/GYN) during preconception planning.1
“The number of women with IBD who are voluntarily childless is startling and worrisome,” comments Sheila E. Crowe, MD, AGAF, AGA Institute past president. “To see that these women are three times more likely than that of the general population to choose not to have a child and to know that many of the reasons for their decisions are rooted in fear, led us to take action.”2,3
New resources to support patients
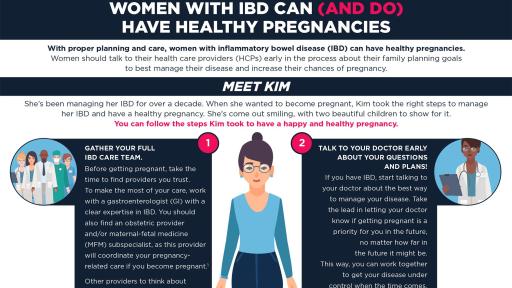
Patients are encouraged to visit the program’s new website, www.IBDParenthoodProject.org, which launched today and houses medical facts about IBD and pregnancy. The website provides answers to common questions and provides a downloadable patient toolkit that features visual and patient-friendly information. Resources include easy-to-digest lists of key questions to ask a provider as women are thinking of becoming pregnant, a flow diagram outlining the various HCPs potentially involved in a woman’s care, a guide to postnatal care and provider locator tools. These tools are a direct response to additional survey findings that reported women with IBD want more and better information about managing their disease.1
“As a proud mother living with IBD, I was drawn to participate in this initiative as I have experienced firsthand how complicated navigating an IBD diagnosis can be in the midst of family planning,” said Jessica Caron, patient advocate. “While I can only wish that these recommendations and resources had been available when I was pregnant, I can work to ensure others don’t go through the same turmoil that I did and that they feel equipped to have these conversations early and often with their health care providers.”
IBD and pregnancy: clinical care pathway guidance
The program comes on the heels of a new clinical care pathway that was published in early 2019 and creates a standardized work flow among HCPs who treat women through conception, pregnancy and after birth. The clinical care pathway was a result of the IBD Parenthood Project Working Group, which was convened in 2018 to drive agreement among providers and offer guidance to those who treat women with IBD.
Understanding the impact of IBD throughout all stages of pregnancy can help HCPs and patients develop a plan to achieve the best outcome and reduce complications. Importantly, for women with IBD, one of the greatest known risks to pregnancy is an IBD flare. The reality is, however, that treating IBD with the appropriate medicine without interruption may help reduce risk of a flare and can help lead to a healthier pregnancy.4 Patients are encouraged to work with their HCPs before they get pregnant, during pregnancy, and after birth to develop and implement a treatment plan and achieve remission. Preconception planning should be a key component for conversations among women of childbearing years and their GI, even if they’re unsure of their future plans. Similarly, an IBD diagnosis should be shared during an initial visit with an obstetric provider.
Among the published recommendations, the care pathway suggests pregnant women with IBD have their care coordinated through an MFM subspecialist, who can determine the type of monitoring needed and frequency of prenatal visits with an obstetric provider, and be followed by a GI with a clear expertise in IBD.4 An MFM is a specially trained obstetrician with an additional three years of formal education and who is board-certified in maternal-fetal medicine, making them highly qualified experts and leaders in the care of complicated pregnancies. An MFM is distinct and different from a “high-risk OB.”5 While some women may not have access to IBD experts and MFM subspecialists, particularly outside of urban centers, any GI, OB/GYN, or specialized physician assistant, nurse practitioner, or midwife can follow the care pathway to help care for women with IBD.
“The new clinical care pathway will give health care providers explicit direction for the treatment and management of women living with this disease,” notes Dr. Uma Mahadevan, AGA spokesperson, IBD Parenthood Project program chair and Professor of Medicine at the Colitis and Crohn’s Disease Center, University of California, San Francisco. “Partnered with the new patient resources available through our program website, we are confident that these pieces will support both patients and HCPs to have open and ongoing dialogue early to promote ideal health for both mom and baby.”
As a trusted voice in the GI community, AGA is dedicated to improving the care of women of childbearing years living with IBD and is committed to redefining industry standards to further standardize and optimize health outcomes for mother, baby and provider. AGA’s IBD Parenthood Project is funded through support from UCB, a global biopharmaceutical company.
About IBD
Inflammatory bowel disease (IBD) is a group of disorders, including Crohn’s disease and ulcerative colitis. These conditions can cause abdominal pain, diarrhea and weight loss. Symptoms can often be controlled by medication, but sometimes surgery is needed, as well. In the U.S., 1.6 million people have IBD. Of those, roughly half are women, and most of them will have the disease during their childbearing years.6,7
The AGA Institute
The American Gastroenterological Association is the trusted voice of the GI community. Founded in 1897, the AGA has grown to more than 16,000 members from around the globe who are involved in all aspects of the science, practice and advancement of gastroenterology. The AGA Institute administers the practice, research and educational programs of the organization. www.gastro.org.
The Crohn’s & Colitis Foundation
The Crohn's & Colitis Foundation is the largest non-profit, voluntary, health organization dedicated to finding cures for inflammatory bowel diseases (IBD). The Foundation’s mission is to cure Crohn's disease and ulcerative colitis, and to improve the quality of life of children and adults who are affected by these diseases. The Foundation works to fulfill its mission by funding research; providing educational resources for patients and their families, medical professionals, and the public; and furnishing supportive services for those afflicted with IBD. For more information visit www.crohnscolitisfoundation.org, call 888-694-8872, or email [email protected].
The Society for Maternal-Fetal Medicine
The Society for Maternal-Fetal Medicine (SMFM) is a non-profit, membership organization based in Washington, DC. With more than 3,500 physicians, scientists and women's health professionals around the world, the Society supports the clinical practice of maternal-fetal medicine by providing education, promoting research and engaging in advocacy to optimize the health of high-risk pregnant women and their babies. SMFM hosts an annual scientific meeting in which new ideas and research related to high-risk pregnancies are unveiled and discussed. For more information, visit www.smfm.org.
Girls With Guts
The vision of Girls With Guts is to establish a national support network that assists women with inflammatory bowel disease (Crohn’s Disease & ulcerative colitis) and/or ostomies in their search for community and acceptance. From in-person events to virtual chats, Girls With Guts provides a variety of programming to bring patients, doctors, and thought leaders together and empower women with IBD through the building of sisterhood and self-esteem. The organization strives to give all women with IBD the strength to find their confidence and keep it, despite having IBD or an ostomy.
UCB
At UCB, everything we do starts with a simple question: "How will this make a difference to the lives of people living with severe diseases?" We have a passionate, long-term commitment to discovering and developing innovative medicines that transform the lives of people living with severe diseases. We do that by connecting with patients and their families around the world living with the physical and social burdens of severe disease. Those connections offer new perspectives, drive innovation, and offer the hope of a new generation of therapies that are helping to transform lives.
BabyCenter
BabyCenter is the world's number one digital parenting resource. Our content reaches more than 100 million people monthly through websites, mobile apps, online communities, email series, social programs, print publications, and public health initiatives. In the United States, 7 in 10 new and expectant moms online use BabyCenter.
We are committed to improving maternal health around the world, and our team works closely with nonprofits, NGOs, and governments to make motherhood safer for all women.
Wakefield Research
Wakefield Research (www.wakefieldresearch.com) is a leading, independent provider of quantitative, qualitative, and hybrid market research. Wakefield Research supports the world’s most prominent brands and agencies, including 50 of the Fortune 100, in 70 countries.
References:
- BabyCenter. 2018. IBD and Preconception, Pregnancy, Early Motherhood.
- Pinder, M., K. Lummis, and C.P. Selinger, Managing inflammatory bowel disease in pregnancy: current perspectives. Clinical and experimental gastroenterology, 2016. 9: p. 325-335.
- Livingston, D., Cohn, D., Childlessness Up Among All Women; Down Among Women with Advanced Degrees, 2010, Pew Research Center.
- Mahadevan et al., Inflammatory Bowel Disease (IBD) in Pregnancy Clinical Care Pathway – A Report from the American Gastroenterological Association IBD Parenthood Project Working Group. Gastroenterology, 2018.
- What is a Maternal-Fetal Medicine Specialist? Society for Maternal-Fetal Medicine. Retrieved October 5, 2018, from https://www.smfm.org/members/what-is-a-mfm.
- Kaplan, G.G. and S.C. Ng, Understanding and Preventing the Global Increase of Inflammatory Bowel Disease. Gastroenterology, 2017. 152(2): p. 313-321 e2.
- Ng, S.C., et al., Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet, 2018. 390(10114): p. 2769-2778.
Contacts:
Monique Dinor
[email protected]
212-292-0418
Aimee Frank
[email protected]
301-941-2620
Download Patient Toolkit
Additional Resources
- IBD Parenthood Project
- Get Your IBD Questions Answered
- What is an MFM?
- Find an IBD Doctor
- Connect with Others